Blog
What is Multidisciplinary Team (MDT) Meeting?
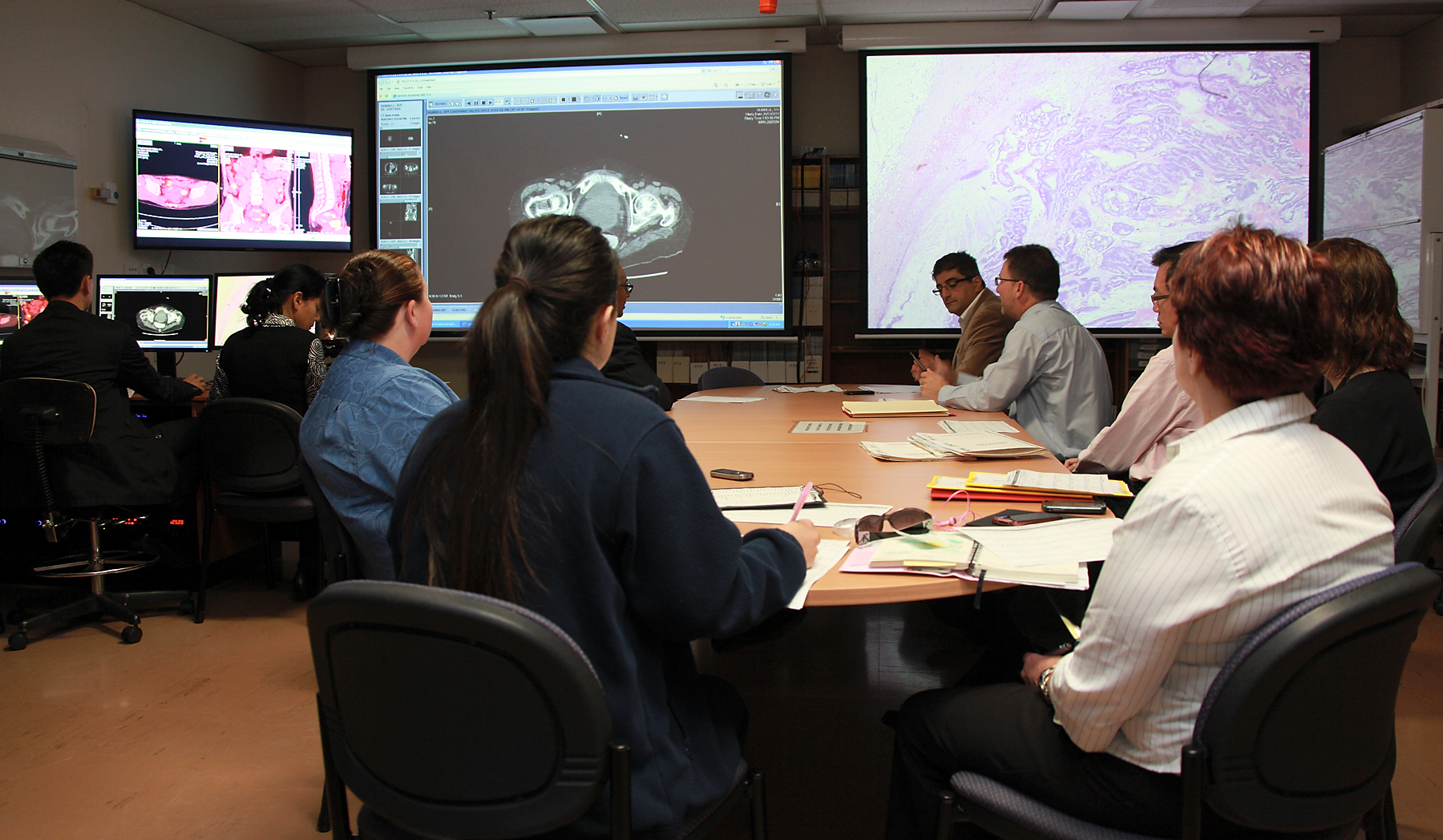
MDT stands for Multidisciplinary Team Meeting. It provides an opportunity for Consultants to discuss complex cases. The principle of an MDT meeting is to discuss patients with other colleagues from the same discipline and where indicates from other specialists in order to ensure the patient is receiving the correct advice and that the treatment is suitable to their individual needs.
The MDT comprises specialist doctors and nurses, who meet regularly to establish that every patient’s diagnosis is correctly made, based on blood and tissue samples, X-rays and scans.
The MDT will then discuss and recommend the best form of treatment based on local and national guidelines and on each individual patient’s circumstances.
MDT meetings may be held at your local hospital, or regionally by video conference to share expertise.
Who attends MDT meetings?
The following core members of the MDT are required to attend meetings every week or fortnight.
Consultant Haematologists and Specialist Registrars who have instigated investigations to obtain a diagnosis and are responsible for the treatment of patients.
Consultant Radiologists who review and report scans and X-rays to confirm diagnosis and who can advise on further testing, monitoring or management.
Consultant Histopathologists who specialise in blood and bone marrow diseases, who report their findings after examining and testing tissue samples to confirm diagnosis.
Consultant Oncologists who recommend and provide radiotherapy treatment when required.
Advanced Nurse Practitioners who ensure that every patient has a named Key Worker allocated and contribute to discussion of care of patients based on holistic needs assessment.
Research Nurse who ensures that any appropriate patients who might benefit from being entered into a clinical trial are discussed.
MDT Coordinator who organises the meetings and ensures the appropriate information is available for cases to be discussed and documented.
Other members of the MDT may not necessarily attend meetings, but are available to provide advice to the MDT and additional care to patients.
These include:
- Specialist Palliative Care Service
- Surgical Services
- Blood and Marrow Transplant (BMT) Service
- Immunologist
- Clinical Psychologist/Psychiatrist
- Occupational Therapist
- Dietitian
- Physiotherapist
- Cancer Pharmacist
- Teenage and Young Adult Cancer Service
Patients may have their cases referred to the MDT at any time, when significant changes occur and further treatment options need to be considered.
The MDT will take into account patients’ views and individual circumstances. The conclusions and recommendations of the MDT are shared with patients at clinic appointments.
Need a comprehensive solution to manage MDT meetings? Please click here
References: